PIM-2 berekening
Coëfficiënten
De PIM-2 risico score wordt berekend met behulp van de volgende coëfficiënten:
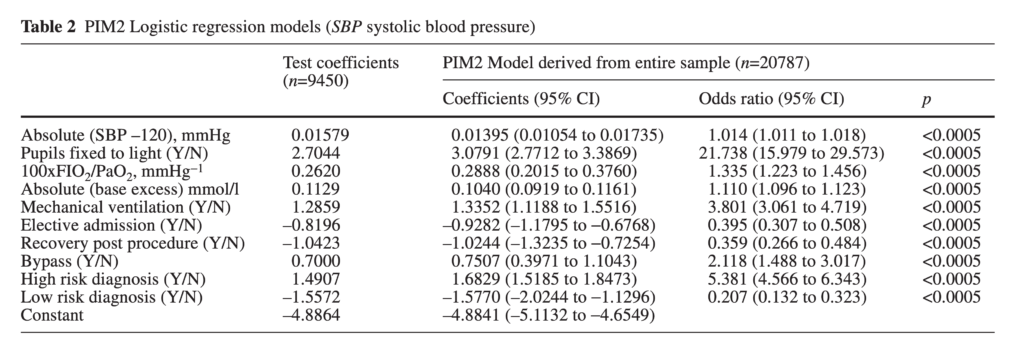
Slater, A., Shann, F., Pearson, G., & Paediatric Index of Mortality PIM Study Group. (2003). PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Medicine, 29(2), 278–285.
Formule
De resulterende regressie formule ziet er dan als volgt uit:
- PIM-2 score =
- -0.9282 x ElectiveAdmission +
- -1.0244 x Recovery +
- 0.7507 x Bypass +
- 1.6829 x HighRisk +
- -1.577 x LowRisk +
- 3.0791 x Pupils +
- 1.3352 x Ventilator +
- 0.01395 x (absolute value of SBP (mmHg) – 120) +
- 0.1040 x (absolute value of BaseExcess (mmol/L)) +
- 0.2888 x (100 x FiO2 / PaO2 (mmHg)) +
- -4.8841
Codering
Ontbrekende waarden worden als volgt gecodeerd:
- ElectiveAdmission = 0
- Recovery = 0
- Bypass = 0
- HighRisk = 0
- LowRisk = 0
- Pupils = 0
- Ventilator = 0
- SBP = 120
- BaseExcess = 0
- Bij ontbreken van FiO2 en/of PaO2:
- FiO2 = 0
- PaO2 = 1
N.B 1 In de PIM-2 worden zowel de laag risico als de hoog risico score meegenomen in de totaal berekening. Dus b.v. een hoog risico diagnose van een hypoplastisch linker hart syndroom in combinatie met een laag risico diagnose van bronchiolitis levert een score op van 1.6829 + -1.577 = 0.1059.
N.B. 2 In de PIM-2 wordt recovery automatisch gescoord indien een bypass operatie heeft plaatsgevonden. Dit resulteert dan in een de-facto score van: -1.0244 + 0.7507 = -0.2737
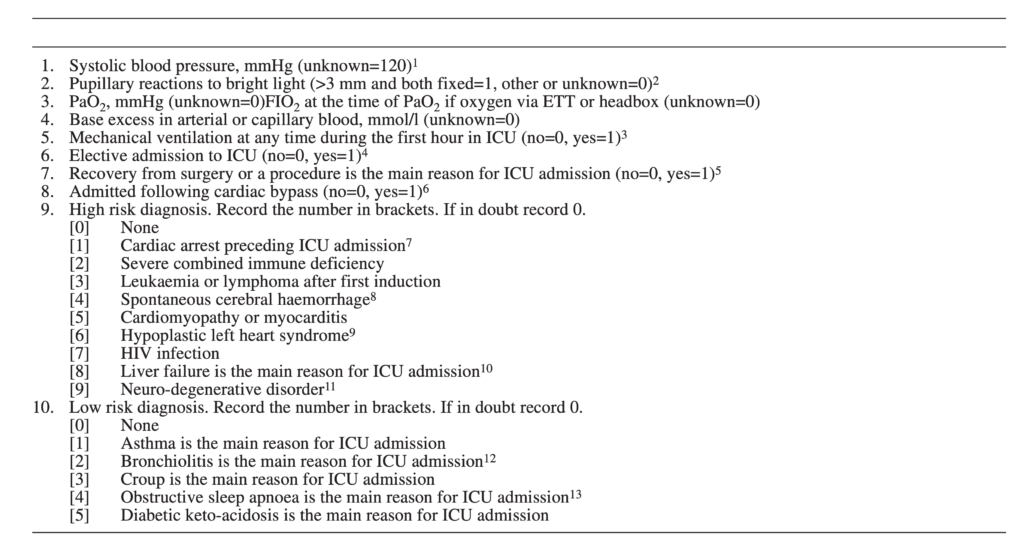
Voor het scoren moeten de volgende regels worden nageleefd:
- Record SBP as 0 if the patient is in cardiac arrest, record 30 if the patient is shocked and the blood pressure is so low that it cannot be measured.
- Pupillary reactions to bright light are used as an index of brain function. Do not record an abnormal finding if this is due to drugs, toxins or local eye injury.
- Mechanical ventilation includes mask or nasal CPAP or BiPAP or negative pressure ventilation.
- Elective admission. Include admission after elective surgery or admission for an elective procedure (e.g. insertion of a central line), or elective monitoring, or review of home ventilation. An ICU admission or an operation is considered elective if it could be postponed for more than 6 h without adverse effect.
- Recovery from surgery or procedure includes a radiology procedure or cardiac catheter. Do not include patients admitted from the operating theatre where recovery from surgery is not the main reason for ICU admission (e.g. a patient with a head injury who is admitted from theatre after insertion of an ICP monitor; in this patient the main reason for ICU admission is the head injury).
- Cardiac bypass. These patients must also be coded as recovery from surgery.
- Cardiac arrest preceding ICU admission includes both in-hospital and out-of-hospital arrests. Requires either documented absent pulse or the requirement for external cardiac compression. Do not include past history of cardiac arrest.
- Cerebral haemorrhage must be spontaneous (e.g. from aneurysm or AV malformation). Do not include traumatic cerebral haemorrhage or intracranial haemorrhage that is not intracerebral (e.g. subdural haemorrhage).
- Hypoplastic left heart syndrome. Any age, but include only cases where a Norwood procedure or equivalent is or was required in the neonatal period to sustain life.
- Liver failure acute or chronic must be the main reason for ICU admission. Include patients admitted for recovery following liver transplantation for acute or chronic liver failure.
- Neuro-degenerative disorder. Requires a history of progressive loss of milestones or a diagnosis where this will inevitably occur.
- Bronchiolitis. Include children who present either with respiratory distress or central apnoea where the clinical diagnosis is bronchiolitis.
- Obstructive sleep apnoea. Include patients admitted following adenoidectomy and/or tonsillectomy in whom obstructive sleep apnoea is the main reason for ICU admission (and code as recovery from surgery).
oorspronkelijke tekst uit: Slater, A., Shann, F., Pearson, G., & Paediatric Index of Mortality PIM Study Group. (2003). PIM2: a revised version of the Paediatric Index of Mortality. Intensive Care Medicine, 29(2), 278–285.
PIM-3 berekening
Coëfficiënten
De PIM-3 score wordt berekend met de volgende coëfficiënten:
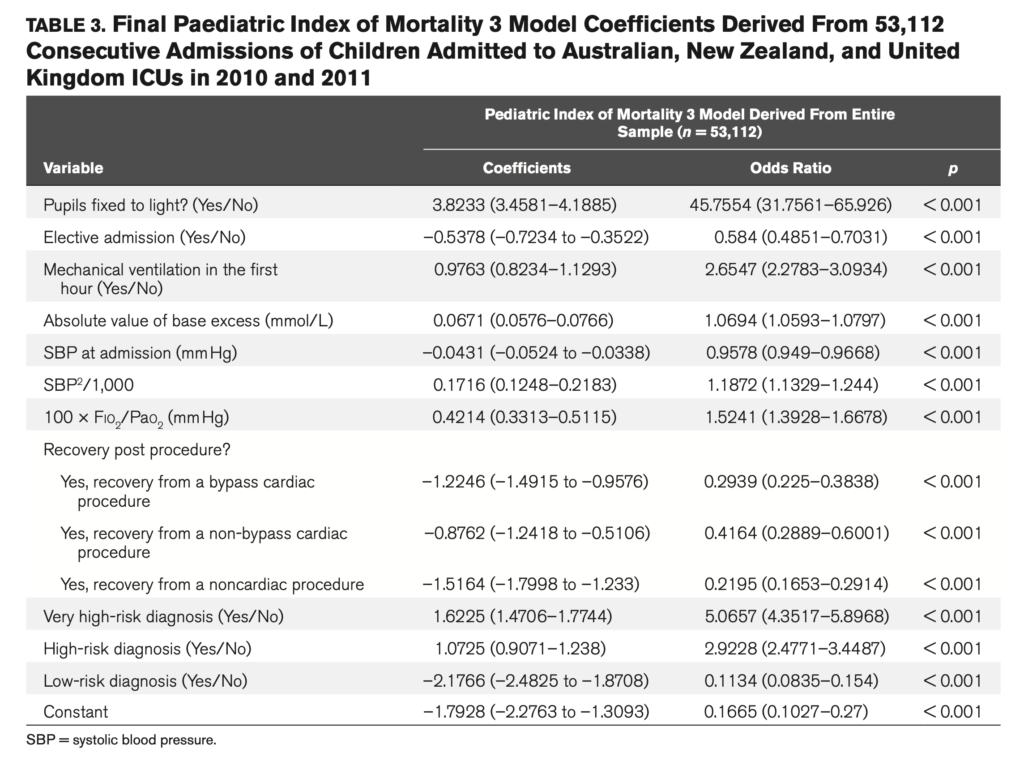
Straney, L., Clements, A., Parslow, R. C., Pearson, G., Shann, F., Alexander, J., & Slater, A. (2013). Paediatric Index of Mortality 3. Pediatric Critical Care Medicine, 14(7), 673–681.
Formule
- PIM-3 score =
- 3.8233 × PupillaryReaction +
- −0.5378 × ElectiveAdmission +
- 0.9763 × MechanicalVentilation +
- 0.0671 × [absolute (BaseExcess)] +
- −0.0431 × SBP + 0.1716 × [SBP2 / 1000] +
- 0.4214 × [(FiO2 × 100) / PaO2] +
- -1.2246 × BypassCardiacProcedure +
- -0.8762 × NonBypassCardiacProcedure +
- -1.5164 × NonCardiacProcedure +
- 1.6225 × VeryHighRisk +
- 1.0725 × HighRisk +
- -2.1766 × LowRisk +
- −1.7928
Codering
Ontbrekende waarden worden als volgt gecodeerd:
- PupillaryReaction = 0
- ElectiveAdmission = 0
- MechanicalVentilation = 0
- BaseExcess = 0
- SBP = 120
- Bij ontbreken van FiO2 en/of PaO2 = 0.23
- Recovery (slechts 1 variabele kan op 1 staan) from:
- BypassCardiacProcedure = 0
- NonBypassCardiacProcedure = 0
- NonCardiacProcedure = 0
- Risk diagnosis (slechts 1 variable kan op 1 staan):
- VeryHighRisk = 0
- HighRisk = 0
- LowRisk = 0
Indien VeryHighRisk = 1 dan HighRisk = 0 en LowRisk = 0. Met andere woorden de diagnose met het hoogste risico wordt in de formule gebruikt. Diagnoses met een lager risico komen dan te vervallen.
Voor het scoren moeten de onderstaande regels worden gevolgd:
PIM-3 is calculated from the information collected at the time a child is admitted to your ICU.
- Record the observations at or about the time of first fact- to-face (not telephone) contact between the patient and a doctor from your ICU (or a doctor from a specialist pediatric transport team).
- Use the first value of each variable measured within the period from the time of first contact to 1 hour after arrival in your ICU. The first contact may be in your ICU, or your emergency department, or a ward in your own hospital, or in another hospital (e.g., on a retrieval).
- Systolic blood pressure, mm Hg (unknown = 120) a
- Pupillary reactions to bright light (> 3mm and both fixed = 1, other or unknown = 0) b
- ([Fio2 × 100] / Pao2). Pao2 mmHg, Fio2 at the time of Pao2 if oxygen via endotracheal tube or headbox (Fio2 or Pao2 unknown, [(Fio2 × 100) / Pao2] = 0.23)
- Base excess in arterial or capillary blood, mmol/L (unknown = 0)
- Mechanical ventilation at any time during the first hour in ICU (no = 0, yes = 1) c
- Elective admission to ICU (no = 0, yes = 1) d
- Recovery from surgery or a procedure is the main reason for ICU admission e
- [0] No
- [1] Yes, recovery from a bypass cardiac procedure
- [2] Yes, recovery from a non-bypass cardiac procedure
- [3] Yes, recovery from a non-cardiac procedure
- Low-riskdiagnosis. If in doubt record 0.
- None
- Asthma is the main reason for ICU admission
- Bronchiolitis is the main reason for ICU admission f
- Croup is the main reason for ICU admission
- Obstructive sleep apnea is the main reason for ICU admission g
- Diabetic ketoacidosis is the main reason for ICU admission
- Seizure disorder is the main reason for ICU admission h
- High-risk diagnosis. If in doubt record 0.
- None
- Spontaneous cerebral hemorrhage i
- Cardiomyopathy or myocarditis
- Hypoplastic left heart syndrome j
- Neurodegenerative disorder k
- Necrotizing enterocolitis is the main reason for ICU admission
- Very high-risk diagnosis. If in doubt record 0.
- None
- Cardiac arrest preceding ICU admission l
- Severe combined immune deficiency
- Leukemia or lymphoma after first induction m
- Bone marrow transplant recipient
- Liver failure is the main reason for ICU admission n
Coding rules. These rules must be followed carefully for PIM3 to perform reliably:
a. Record SBP as 0 if the patient is in cardiac arrest; record 30 if the patient is shocked and the blood pressure is so low that it cannot be measured.
b. Pupillary reactions to bright light are used as an index of brain function. Do not record an abnormal finding if this is due to drugs, toxins, or local eye injury.
c. Mechanical ventilation includes invasive ventilation, mask or nasal continuous positive airway pressure, or bilevel positive airway pressure, or negative pressure ventilation.
d. Elective admission. Include admission (planned or foreseeable) after elective surgery or admission for an elective procedure (e.g., insertion of a central catheter), or elective monitoring, or review of home ventilation. An ICU admission or an operation is considered elective if it could be postponed for more than 6 hours without adverse effect.
e. Recovery from surgery or procedure (includes a radiology procedure or cardiac catheter). Do not include patients admitted from the operating theater where recovery from surgery is not the main reason for ICU admission (e.g., a patient with a head injury who is admitted from theater after insertion of an intracranial pressure monitor; in this patient the main reason for ICU admission is the head injury).
f. Bronchiolitis. Include children who present either with respiratory distress or central apnea where the clinical diagnosis is bronchiolitis.
g. Obstructive sleep apnea. Include patients admitted following adenoidectomy and/or tonsillectomy in whom obstructive sleep apnea is the main reason for ICU admission (and code as recovery from surgery).
h. Seizure disorder. Include patients who require admission primarily due to status epilepticus, epilepsy, febrile convulsion, or other epileptic syndrome where admission is required either to control seizures or to recover from the effects of seizures or treatment.
i. Cerebral hemorrhage must be spontaneous (e.g., from aneurysm or AV malformation). Do not include traumatic cerebral hemorrhage or intracranial hemorrhage that is not intracerebral (e.g., subdural hemorrhage).
j. Hypoplastic left heart syndrome. Any age, but include only cases where a Norwood procedure or equivalent is required in the neonatal period to sustain life.
k. Neurodegenerative disorder. Requires a history of progressive loss of milestones (even if no specific condition has been diagnosed), or a diagnosis where this will inevitably occur.
l. Cardiac arrest preceding ICU admission includes both in-hospital and out-of-hospital arrest. Requires either documented absent pulse or the requirement for external cardiac compression. Do not include past history of cardiac arrest.
m. Leukemia or lymphoma. Include only cases where admission is related to leukemia or lymphoma or the therapy for these conditions.
n. Liver failure, acute or chronic. Must be the main reason for ICU admission. Do not include patients admitted following an elective liver transplant.
Oorspronkelijke tekst uit: Straney, L., Clements, A., Parslow, R. C., Pearson, G., Shann, F., Alexander, J., & Slater, A. (2013). Paediatric Index of Mortality 3. Pediatric Critical Care Medicine, 14(7), 673–681.
PRISM-IV berekening
Coëfficiënten
De PRISM-IV wordt berekend met de volgende coëfficiënten:
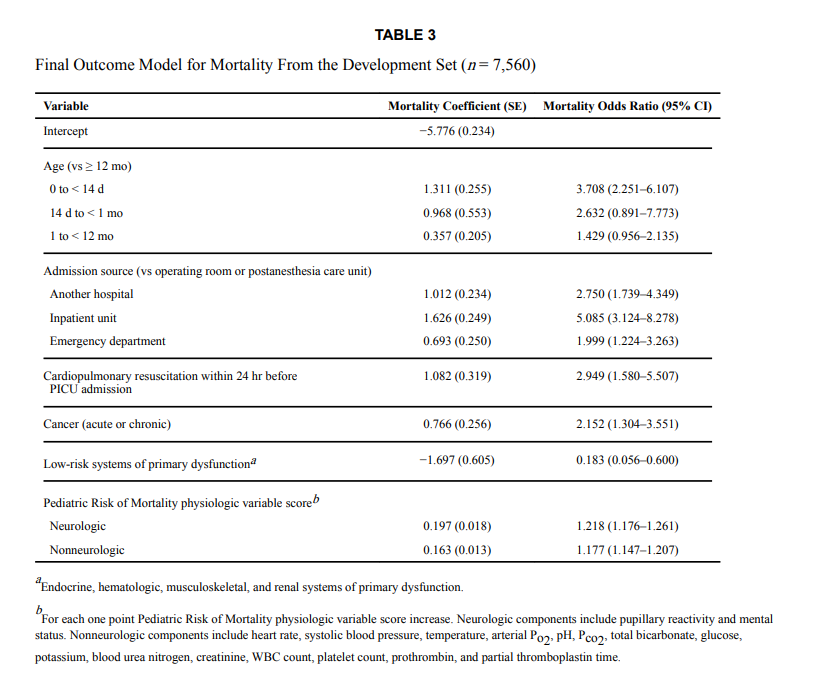
PRISM-III score tabel
De neurologische en niet-neurologische score wordt berekend met behulp van onderstaande score tabel.
| Bepaling | Leeftijd | Range | Score |
|---|---|---|---|
| Systolische Bloeddruk (mmHg) | 0 – 1 maand | 40 – 55 | 3 |
| 1 maand – 1 jaar | 45 – 65 | ||
| 1 jaar – 12 jaar | 55 – 75 | ||
| > 12 jaar | 65 – 85 | ||
| 0 – 1 maand | < 40 | 7 | |
| 1 maand – 1 jaar | < 45 | ||
| 1 jaar – 12 jaar | < 55 | ||
| > 12 jaar | < 65 | ||
| Hart actie (aantal/min) | 0 – 1 maand | 215 – 225 | 3 |
| 1 maand – 1 jaar | 215 – 225 | ||
| 1 jaar – 12 jaar | 185 – 205 | ||
| > 12 jaar | 145 – 155 | ||
| 0 – 1 maand | > 225 | 4 | |
| 1 maand – 1 jaar | > 225 | ||
| 1 jaar – 12 jaar | > 205 | ||
| > 12 jaar | > 155 | ||
| Temperatuur (Celsius) | alle leeftijden | < 33 of > 40 | 3 |
| Acidose (bicarbonaat in mmol/L) | alle leeftijden | pH 7.0 – 7.28 of bicarbonaat 5 – 16.9 | 2 |
| pH < 7.0 of bicarbonaat < 5 | 6 | ||
| Bicarbonaat (mmol/L) | alle leeftijden | > 34 | 4 |
| pH | alle leeftijden | 7.48 – 7.55 | 2 |
| > 7.55 | 3 | ||
| PaO2 (mmHg) | alle leeftijden | 42.0 – 49.9 | 3 |
| < 42 | 6 | ||
| PCO2 (mmHg) | alle leeftijden | 50 – 75 | 1 |
| > 75 | 3 | ||
| Glucose (mmol/L) | alle leeftijden | > 11 | 2 |
| Kalium (mmol/L) | alle leeftijden | > 6.9 | 3 |
| Kreatinine (micromol/L) | 0 – 1 maand | > 75 | 2 |
| 1 maand – 1 jaar | > 80 | ||
| 1 jaar – 12 jaar | > 80 | ||
| > 12 jaar | > 115 | ||
| Ureum (mmol/L) | 0 – 1 maand | > 4.3 | 3 |
| > 1 maand | > 5.4 | ||
| Leukocyten (10^9/L) | alle leeftijden | < 3 | 4 |
| PT of PTT (seconden) | 0 – 1 maand | PT > 22 of PTT > 85 | 3 |
| > 1 maand | PT > 22 of PTT > 57 | ||
| Trombocyten (10^9/L) | alle leeftijden | 100 – 200 | 2 |
| 50 – 100 | 4 | ||
| < 50 | 5 | ||
| NIET NEUROLOGISCHE | Totaal | ||
| Pupil reflex | alle leeftijden | 1 gefixeerd | 7 |
| beiden gefixeerd | 11 | ||
| Bewustzijn | alle leeftijden | GCS < 8 | 5 |
| NEUROLOGISCHE | Totaal |
Een oorspronkelijke handleiding voor het scoren van de PRISM-III kan hier worden geopend: PRISM(3)-definities
Online calculators
Voor de PIM-2 zijn 2 online calculators te vinden:
Voor de PIM-3 is een calculator online van de ESPNIC beschikbaar.
Voor de PRISM zijn de volgende online calculators beschikbaar:
